Back Surgery Article – Dr Singh, Dr Hsu, Dr Farey
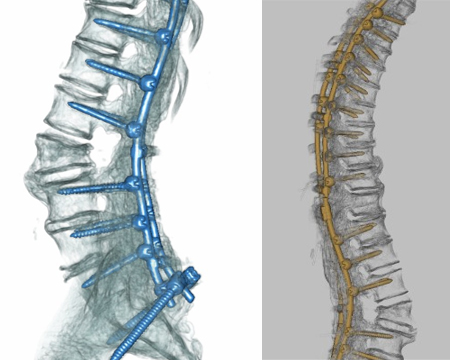
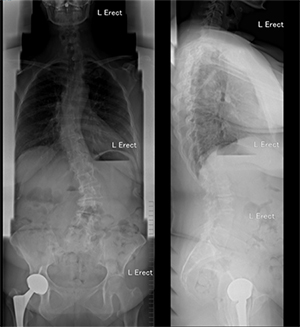
Dual-Surgeon Spinal Deformity Surgery
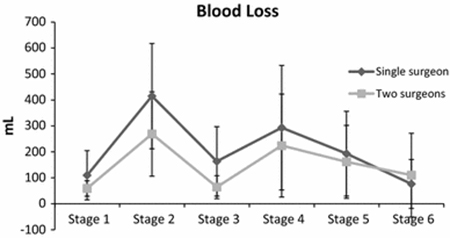
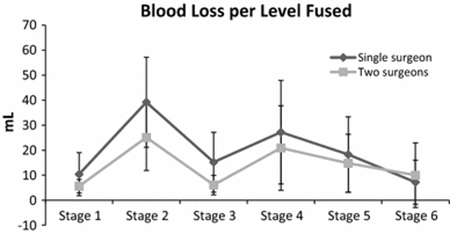
Deformity surgery is one of the more challenging procedures in spinal surgery and can account for long operative times and blood losses. Even among Fellowship-trained Deformity Surgeons, many studies show intraoperative adverse events and related postoperative complications rate of 10 to 15%. Significant blood loss in posterior spinal fusion (PSF) surgery for paediatric and adult scoliosis can cause haemodynamic complications and increases the incidence of allogeneic blood transfusion. The increased risk of intra-operative bleeding is related to the long incision, extensive soft tissue dissection, multi-level decompression surgery, decortication of bony surfaces and prolonged operative time.
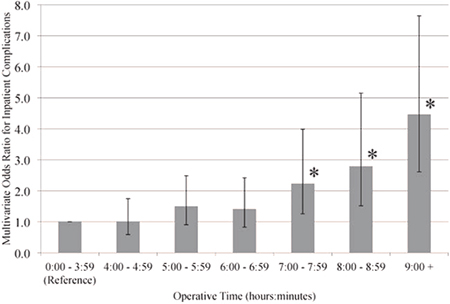
Allogenic blood transfusion and increased operative times have been associated with increased infection rate (Shen et al). Surgical site infections (SSI) in spinal deformity surgery carry a very high morbidity to the patient, the family, and a high cost to society. Operative time greater than 5 hours has been associated with higher rates of infection.
| Table 1: Typical Surgical stages in spine deformity surgery: | ||
| Stage 1 | Exposure | Time taken for skin incision, dissection of subcutaneous tissue and paravertebral muscles to expose the posterior surface of the vertebrae |
| Stage 2 | Screws insertion | Time taken to insert all the pedicle screws planned from the upper to the lowest instrumented vertebra |
| Stage 3 | Release and decompression | Time taken for all facetectomies and osteotomies and decompression of neural elements |
| Stage 4 | Correction | Time taken for insertion of the rods, correction of the deformity |
| Stage 5 | Corticotomies and bone grafting | Time taken for corticotomies of the posterior vertebral laminae and transverse processes and laying morcelized local bone grafts |
| Stage 6 | Closure | Time taken to close the fascia, subcutaneous tissue and skin |
To date, many strategies have been in use to attempt to reduce perioperative complications in adult deformity surgery. These include better preoperative planning strategies, intraoperative neuromonitoring, having a blood transfusion/cell saver strategy and staging surgeries.
The utility and efficacy of 2 consultant surgeons working simultaneously has been described in the literature for procedures such as bilateral anterior cruciate ligament reconstruction, laparoscopic nephrectomy, breast surgery and esophagectomy.
Similar results were found in complex spine surgery studies. Halanski et al, Ames et al, Chan et al. reported that the involvement of two surgeons in corrective surgery for scoliosis was associated with reduced operative time, blood loss and the need for allogenic blood transfusion.
The Seattle spine team found that other complication rates were significantly lower as well when two consultant-level surgeons operated simultaneously on cases involving long fusions (16% vs. 52%). There were significantly lower return rates to the operating room during the perioperative 90-day period (0.8% vs. 12.5%), lower rates of wound infection requiring debridement (1.6% vs. 7.5%), lower rates of deep vein thrombosis/pulmonary embolism (3.2% vs. 10%), and lower rates of postoperative neurological complications (0.5% vs. 2.5%). The use of 2 surgeons experienced in spine deformity also helped achieve a decreased rate in major complications, decreased rate in premature case termination, and decreased rate of returns to the operating room within 30 days.
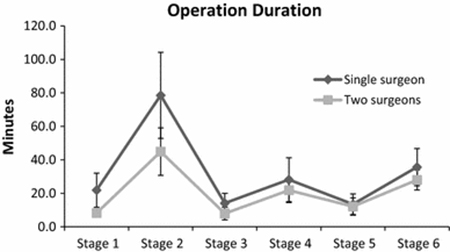
The mean operating time reported in literature for adult spinal deformity surgery involving 5 or more levels is around 300 to 360 minutes. Reducing operating time while maintaining strict adherence to good surgical technique and avoidance of intraoperative complications is key to good outcome for patients.
Since 2008, two of the authors have been performing Dual-Surgeon Deformity Surgery (DSDS) at North Shore Private Hospital. Over the last 10 years, with the additional of our third author in 2014, we have performed over 500 Dual-Surgeon procedures at North Shore Private Hospital. There has been no deep infections that required return to theatre in the DSDS group. The average surgical time is less than 4 hours and 25 minutes.
Pre-operative planning plays a major role in reducing surgical time and achieving maximum efficiency in the operating theatre. The surgical team is comprised of regular members of nursing and anaesthetic staff who are experience in all the different aspects of DSDS and are able to coordinate multiple tasks efficiently.
Surgery is performed in both a simultaneous and tandem manner. Each patient’s procedure is tailored to their anatomy and their needs, and different steps of the operation (such as decompression, osteotomies, correction and screw placement) are simultaneously carried out in concert. The surgical team needs to be able to cater to two surgeons performing different steps of the operation at the same time.
DSDS technique has been successful in safely minimizing overall operative time while achieving the surgical goal with a reduced infection rate.



References:
- Ames CP, Barry JJ, Keshavarzi S, Dede O, Weber MH, Deviren V (2013) Perioperative outcomes and complications of pedicle subtraction osteotomy in cases with single versus two attending surgeons. Spine Deform 1(1):51–58.
- Single vs two attending senior surgeons: assessment of intra- operative blood loss at different surgical stages of posterior spinal fusion surgery in Lenke 1 and 2 adolescent idiopathic scoliosis Mun Keong Kwan • Chee Kidd Chiu • Chris Yin Wei Chan Eur Spine J (2017) 26:155–161
- Halanski MA, Elfman CM, Cassidy JA, Hassan NE, Sund SA, Noonan KJ (2013) Comparing results of posterior spine fusion in patients with AIS: are two surgeons better than one? J Orthop 10:54–58
- Chan CY, Kwan MK (2015) Peri-operative outcome in posterior spinal fusion for adolescent idiopathic scoliosis: a prospective study comparing single versus two attending surgeons strategy. Spine (Phila Pa 1976)
- The Seattle Spine Team Approach to Adult Deformity Surgery: A Systems-Based Approach to Perioperative Care and Subsequent Reduction in Perioperative Complication Rates
Spine Deformity, Volume 2, Issue 2, March 2014, Pages 95-103 - Rampersaud Y.R., Moro E.R., Neary M.A., et al: Intraoperative adverse events and related postoperative complications in spine surgery: implications for enhancing patient safety founded on evidence-based protocols. Spine (Phila Pa 1976) 2006; 31: pp. 1503-1510
- Shen J, et al. Risk factors for delayed infections after spinal fusion and instrumentation in patients with scoliosis. J Neurosurg Spine 2014 Oct;21(4):648-52. doi: 10.3171/2014.6.SPINE13636. Epub 2014 Jul 4
 Menu
Menu